Seminars
Title: A New Era of Care Delivery: Machine-learning Enhanced Hospital Workload Prediction and Resource Allocation
Speaker: Dr. Pengyi Shi, Operations Management at the Krannert School of Management, Purdue University
Time: 10:00 am EST, April 27
Modality: Virtual
Zoom information: https://virginiatech.zoom.us/j/5569243852
YouTube link: https://youtu.be/rO8myNYBJsY
If you plan to attend, please fill this short registration form: https://forms.gle/k3hdmqnsoUPJTn577
Abstract:
The COVID-19 pandemic has created new opportunities to develop and deploy high-impact analytics to combat severe resource shortages in a rapidly evolving environment. Nursing organizations suffered both during and in the aftermath of the pandemic from excess demand for and diminishing supply of nurses. Staffing inadequacy leads to high nurse burnout and turnover, decreased quality of care, worse patient outcomes, and enlarged disparity in health access. At the core of solving these issues are comprehensive, data-based analytics and predictions to understand: (i) the patient workload; (ii) how to most efficiently allocate resources to all patients; and (iii) how to effectively create surge capacity in response to resource shortage. In this research, we leverage a suite of analytics tools to develop an integrated, comprehensive solution to support decisions on all these aspects. Specifically, we develop novel machine-learning-based occupancy forecasting models that account for different patient acuity levels. Using distributional information from this forecast, we generate workload scenarios for the hospital network, which then are fed into a two-stage stochastic program to support nurse deployment and surge planning decisions. Based on a close partnership with IU Health System, the largest health system in Indiana with 16 hospitals, we launched an academia-industry venture to implement and deploy our data-driven solution. The tool was gone live as a pilot in October 2021. We logged the performance of the recommendations from October 2021 to March 2022 as proof of value. Analysis indicates system-wide improvements in all metrics: with reductions of 5% understaffing, 3% misallocation of resource nurses, and 1% overstaffing, with an estimated annual savings of over $300K.
Bio:
Dr. Pengyi Shi is an associate professor at the Krannert School of Management, Purdue University. She received her Ph.D. degree in Industrial Engineering from Georgia Institute of Technology before joining Purdue in 2014. Her research interests include data-driven modeling and decision-making in healthcare and service operations. She has collaborated with practitioners and faculty members from different healthcare organizations, including major hospitals in the US, Singapore, and China. Her research has won the first place of MSOM Responsible Research in OM Award in 2021, the first place of INFORMS Pierskalla Best Paper Award in 2018, and the second place of POMS CHOM Best Paper Award in 2019 and 2020.
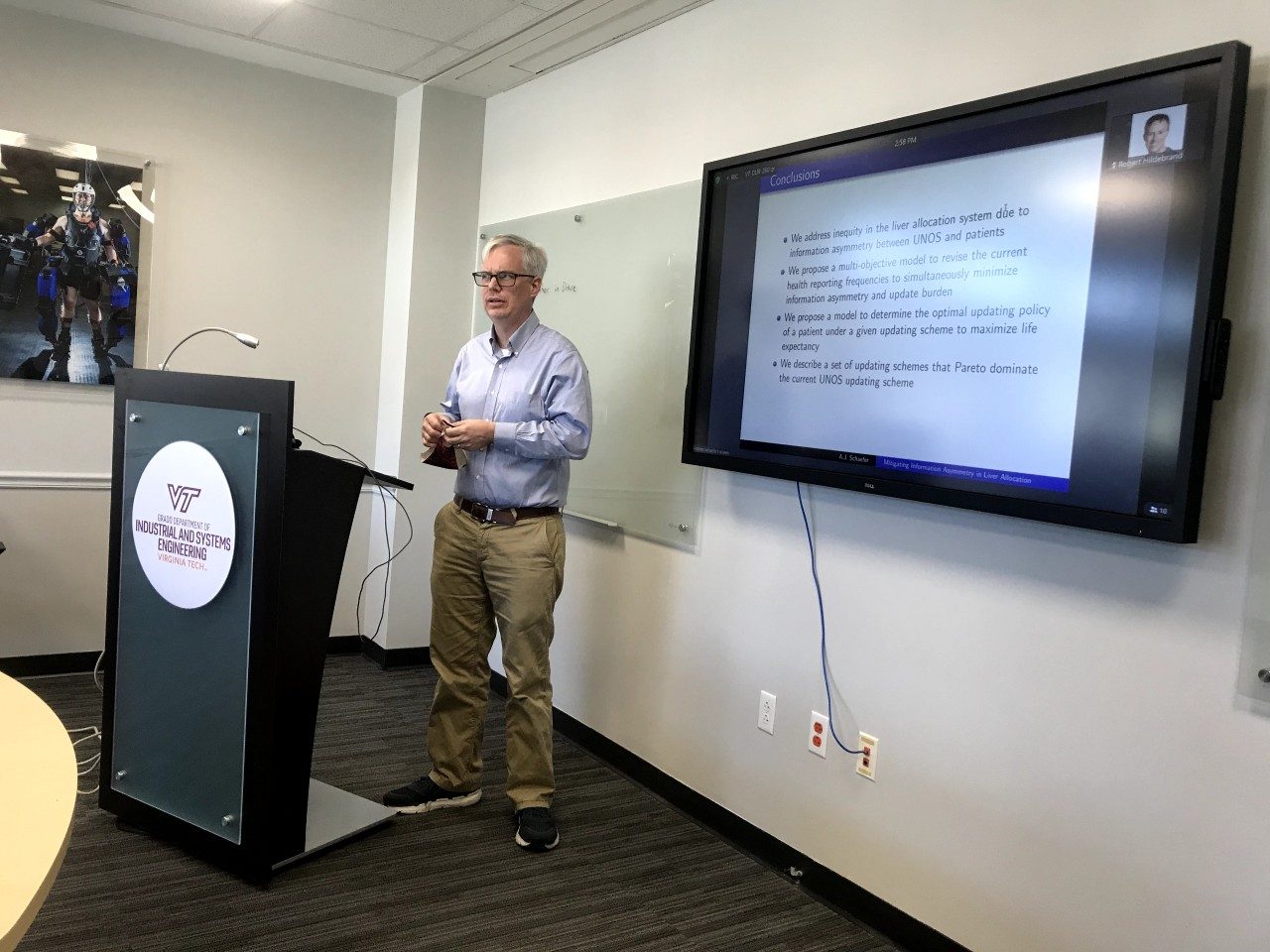
Title: Mitigating Information Asymmetry in Liver Allocation
Speaker: Dr. Andrew Schaefer, Computational and Applied Mathematics at Rice University
Time: 2:00 pm EST, March 28
Modality: Both in-person and virtual available (see details below)
In-person Location: Durham 260
Zoom information: https://virginiatech.zoom.us/j/5569243852
Recording: https://youtu.be/195-1tAkgLg
If you plan to attend, please fill this short registration form: https://forms.gle/uryJ2uHcufLXv9Kg9
Abstract:
In accordance with the National Organ Transplant Act (NOTA), which requires the efficient and equitable allocation of donated organs, the United Network for Organ Sharing (UNOS) prioritizes patients on the liver-transplant waiting list within given geographic areas based mainly on their most recently reported health status. Accordingly, UNOS requires patients to update their health status at a frequency that depends on their last reported health status. However, patients may elect to update any time within the required timeframe, which creates opportunities to game the system, leading to information asymmetries between UNOS and the patients on the waiting list. This information asymmetry can be alleviated through more frequent updating requirements, but at the price of an increased update burden (e.g., data collection costs and patient inconvenience).
We propose a model that determines health reporting requirements that simultaneously minimize these two (possibly conflicting) criteria, i.e., inequity due to information asymmetry and update burden. Calibrating the model with clinical data, we examine (1) the degree to which an individual patient can benefit from the flexibility inherent to the current health reporting requirements, and (2) alternative recommendations that dominate the current requirements with respect to the two criteria of interest.
This is joint work with Sepehr Nemati, Zeynep Icten and Lisa Maillart.
Bio:
Dr. Andrew Schaefer is Noah Harding Chair and Professor of Computational and Applied Mathematics at Rice University. He received his PhD in Industrial and Systems Engineering from Georgia Tech in 2000. His research interests include stochastic optimization methodology and its application to health care problems. In particular, he is interested in optimizing decisions arising in the treatment of a variety of diseases, including end-stage liver disease, HIV/AIDS, influenza, and cancer.
Title: Designing Healthcare for Human Use: ISE, Human Factors, and Application in Healthcare
Time: 3:30 pm EST, January 27
Location: Durham 260 (and Zoom)
Zoom information: https://virginiatech.zoom.us/j/5569243852
Abstract:
As healthcare has continued to increase in complexity, the need for systems engineering has only grown. In this talk, I will discuss selected research projects that have merged systems engineering and human factors to address challenging healthcare processes and outcome problems. Specifically, I will focus on projects in the operating room, process improvement projects within healthcare, and finally community/public health challenges. I will discuss opportunities for ISE in health and healthcare.
Bio:
Dr. Sarah Parker is the Chair of Health Systems and Implementation Science at Virginia Tech Carilion School of Medicine. She has over 15 years of experience applying human factors and industrial/organizational psychology principles to healthcare. Sarah Parker received her BA in psychology from Wittenberg University in Springfield OH and her MA in human factors and applied cognition from George Mason University in Fairfax VA. Prior to pursuing her PhD, she worked at Mayo Clinic applying human factors principles to various inpatient quality and safety challenges. She then pursued her PhD at University of Aberdeen in Scotland. She was a Ruth L. Kirschstein Post Doctoral Fellow, focusing on team coordination during trauma resuscitation. Her research has been funded by the NIH, the Robert Wood Johnson Foundation, and many other local and national foundations. Dr. Parker’s research interests include team performance and communication in high risk settings, applying innovative methods to better understand human performance, implementation science and using human centered design to improve healthcare delivery. She has presented at numerous national and international conference and published over 50 peer reviewed articles and book chapters on human factors and patient safety. Most importantly, Dr. Parker and her husband Michael are parents of Layla, Jack and Miles.
Title: The Impact of Vertical Integration on Physician Behavior and Healthcare Delivery: Evidence from Gastroenterology Practices
Abstract:
The U.S. healthcare system is undergoing a period of substantial change, with hospitals purchasing many physician practices (“vertical integration”). In theory, this vertical integration could improve quality by promoting care coordination, but could also worsen it by impacting the care delivery patterns. The evidence quantifying these effects is limited, because of the lack of understanding of how physicians’ behaviors alter in response to the changes in financial ownership and incentive structures of the integrated organizations. We study the impact of vertical integration by examining Medicare patients treated by gastroenterologists, a specialty with a large outpatient volume, and a recent increase in vertical integration. Using a causal model and large-scale patient-level national panel data that includes 2.6 million patient visits across 5,488 physicians between 2008-2015, we examine changes in various measures of care delivery, including care processes, patient outcomes, operational efficiency, and spending. We find that physicians significantly alter their care process (e.g., in using anesthesia with deep sedation) after they vertically integrate, which in turn results in a substantial increase in patients’ post-procedure complications. We further provide evidence that the financial incentive structure of the integrated practices is the main reason for the changes in physician behavior, since it discourages the integrated practices from allocating expensive resources to relatively unprofitable procedures. We also find that although integration improves operational efficiency (measured by physicians’ throughput), it negatively affects quality and overall spending. Finally, to shed light on potential mechanisms through which policymakers can mitigate the negative consequences of vertical integration, we perform both mediation and cost-effectiveness analyses. Our results indicate that additional payment for encouraging the use of deep sedation, up to the price that is 150% of the current price for a colonoscopy alone, for providing deep sedation during colonoscopy, can be viewed as a cost-effective mechanism to prevent the vertical integration trends from degrading the quality of care.
Title: Diseases and Dysfunctions of the Fourth Dimension: Challenges and Opportunities of a New Healthcare Frontier
Abstract:
Over the last century, the causes of ill health have increasingly resulted from our own behavior. Undergirding this ill health is a foreshortened time horizon -- largely unrecognized in healthcare systems. Time horizon, depending upon its length, enhances and diminishes the value of different health and ill health producing behaviors. By not recognizing the contribution to health and ill health of a patient’s time horizon, health systems may fail to help the patient. In this talk, time horizon’s determinants, interventions for time horizon and its impact on health behaviors, and the implications for health systems will be described and discussed.